This is the third edition of The 2 Susans, a monthly LinkedIn newsletter produced by Dr. Susan Baumgaertel and Dr. Susan Vogler.
We are two doctors who are curious about aging. Our newsletter embraces conversations about aging from many different perspectives—medical, psychological, societal and even personal. Of course we’ll have a lot of content that pertains to peri/menopause and beyond.
To read the May edition, click here. To read this new edition on LinkedIn, click here.
Enjoy the reprint below!
Cancer Support, Risk & Screening
How fitting that I talk about my own cancer story this month. In keeping with this twist (doctor becomes patient), instead of the usual tips for navigating cancer you’ll learn the top four things NOT to say to someone with a new cancer diagnosis. You’ll also get a refresher on cancer risk/reduction and screening from my esteemed colleague Dr. Vogler.
Susan B:
As we age, the risk of most cancers increases. It becomes important in midlife to pay attention to screening recommendations—don’t skip that annual exam!
The proverbial tables were turned for me earlier this year when I was diagnosed with cancer. After three decades of caring for my patients with cancer it was “my turn.” Over the years I’d been asked many times, “What would you do if you had my cancer?” My answer was always the same—I wouldn’t know unless I actually had cancer.
Support for someone going through cancer treatment can be quite nuanced, especially depending on where they are at in their journey. I’ve often reflected on the myriad ways to approach support, and even collected my thoughts in video format: I Have Cancer, Now What?
What you don’t often find, however, is instruction on what not to do or not to say. Here are a few tips to consider, based solely on my personal experience.
- What kind of cancer? When someone has just told you they have cancer, repress the urge to immediately ask what kind of cancer they have. They are likely in a vulnerable position and not ready for the “20 questions” game. Yes, there is a huge difference between basal cell skin cancer and metastatic pancreatic cancer. But, it is their story to tell, not your list to check off. Give them time and space.
- My uncle had that same cancer! Who cares? Seriously, it may sound to you like you are empathizing and identifying with their journey, but telling someone who’s just revealed to you they have cancer that you know someone else who had it too is tone deaf. It’s not a competition.
- Will you be getting chemo? Although you might be considering batch-cooking lasagna to provide support, jumping right into treatment questions can be off-putting. The best approach is just to listen and take cues. You’ll be able to better understand their journey over time. You don’t need all the facts up front to provide support.
- Surgery is the cure! While statistically that might be true, saying that to a patient can be a bit dismissive. I understand that a physician desires to give their patients hope—I used to say that too. But, even though my cancer has great outcomes, there was still a 5% chance of recurrence and/or metastatic disease. That was vastly different than a cure. I was able to get my brain around this and embrace my new mantra “I am cured,” but it took time to get there.
I’m happy to say that I am now a cancer survivor. It does take a team. It is also a very personal journey. For those who need additional resources please visit my favorite nonprofit, Cancer Lifeline—free support for all who are touched by cancer. Because no one should go through cancer alone.
I celebrate all cancer survivors this month!

Neighborhood flowers in Seattle. Photo credit: Dr. Susan Baumgaertel, April 10, 2024.
Susan V:
Although the cancer death rate has been on the decline, new cancer cases are on the rise, according to the American Cancer Society. The people most likely to be diagnosed with cancer are 65 and older. In 2023, there were over 2 million new cases, that is over 5000 cancer cases per day; by 2050, researchers estimate there will be 35 million new cases. That’s huge. The increase is partly due to an aging US population, and other risk factors such as tobacco, alcohol, consumption of ultra-processed foods, obesity, and pollution are also to blame. But that’s not all because there’s more to this picture. It’s about the younger population, people aged 50 years or younger, who are being diagnosed with cancer.
Some types of cancers are rising among young people, such as colorectal cancer, breast cancer, and uterine cancer. Screening for these cancers at an earlier age is vital to detect and treat cancer early before it spreads and hence increase the chance for survival. Medical experts now recommend that average-risk individuals have colorectal screening with colonoscopy starting at 45 years of age. A yearly mammogram starting at age 40 is essential, and prompt medical evaluation with examination, imaging, and biopsy is critical in detecting high-grade precancerous and cancerous cells. Access to medical care, regardless of age, race, and background, is crucial in recognizing the development of cancer.
There’s a lot of talk about genetic testing. The BRCA test may be the most talked about genetic test in the news and social media. Doctors recommend the BRCA genetic test to women with a strong family history of cancer, such as breast and ovarian cancers. When the BRCA test is positive, implementation of more frequent and comprehensive breast imaging and ovarian cancer surveillance, as well as consideration for surgery, significantly lowers risk.
According to the CDC, researchers have found at least 13 cancers related to obesity, including colorectal, breast, ovarian, and uterine, and these 13 cancers make up 40 % of all cancers! Obesity is associated with increased circulating hormones and prolonged-lasting inflammation, and these changes can lead to cancer. Maintain optimal body weight with proper exercise and a diet rich in whole grains, legumes, lean meat, fruits, and vegetables. Avoid processed foods and alcohol.
Cancer deaths are on the decline, and this is good news because more people are surviving cancer. And despite this, being diagnosed with cancer can be devastating and heart-wrenching for many, including family members. My Mom was diagnosed with non-Hodgkin’s Lymphoma during my 3rd year of medical school while studying the hematology/oncology curriculum. It was a difficult time, to say the least, but what I remember most was the support of her medical team members, especially her oncologist, who would always o]er encouraging words.
I celebrate all cancer survivors, and I honor Dr. Susan B. for her courage in battling cancer, and I congratulate her for the battle she won.
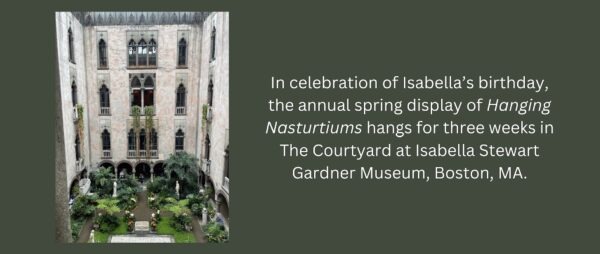
Flowers at Boston museum. Photo credit: Dr. Susan Vogler, March 29, 2024.
🗓️ Our July edition is coming soon: “Stars & Stripes: Beyond Body Image.”
📝💬 The 2 Susans would love to hear from you!
Let us know the aging topics YOU are curious about. Please also share this newsletter in your network and tag us—we are so grateful.
Susan B: susan@mymdadvocate.com
LinkedIn, myMDadvocate, MenopauseMenu, The Menopause Menu book
Susan V: susan@voglermedical.com
The 2 Susans newsletter is for informational purposes only. It does not represent medical advice and is not intended as a substitute for professional advice, diagnosis, or treatment. Always consult with your private physician.